
The U.S. Food and Drug Administration on Friday approved the country’s first gene-editing treatment, Casgevy, for use in patients with sickle cell disease.
The approval comes about a decade after the discovery of CRISPR technology for editing human DNA, representing a significant scientific advancement. Yet reaching the tens of thousands of people who could benefit from the treatment could be challenging given the potential hurdles — including cost, at $2.2 million per patient — of administering the complex therapy.
Casgevy, co-developed by Vertex Pharmaceuticals and CRISPR Therapeutics, uses Nobel Prize-winning technology CRISPR to edit a person’s genes to treat disease. The treatment was approved by U.K. regulators last month.
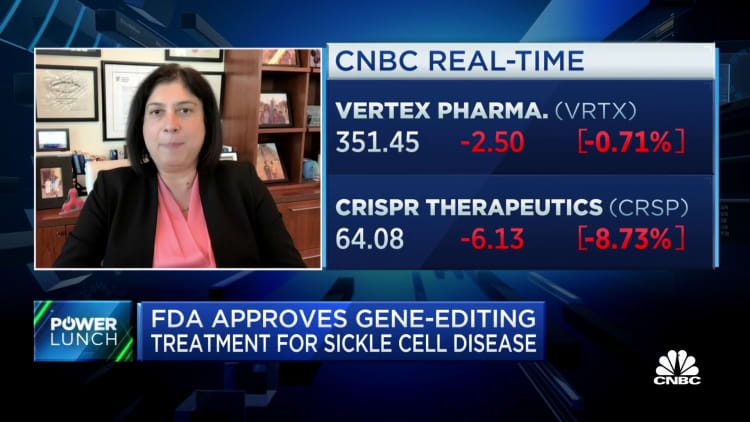
Shares of Vertex fell 1% Friday, while shares of CRISPR fell 8%.
Sickle cell, an inherited blood disorder, causes red blood cells to become misshapen half moons that get stuck inside blood vessels, restricting blood flow and causing what are known as pain crises. About 100,000 Americans are estimated to have the disease.
This microscope photo provided on Oct. 25, 2023, by the Centers for Disease Control and Prevention shows crescent-shaped red blood cells from a sickle cell disease patient in 1972. Britain’s medicines regulator has authorized the world’s first gene therapy treatment for sickle cell disease, in a move that could offer relief to thousands of people with the crippling disease in the U.K.
Dr. F. Gilbert/CDC via AP, File
Casgevy uses CRISPR to make an edit to a person’s DNA that turns on fetal hemoglobin, a protein that normally shuts off shortly after birth, to help red blood cells keep their healthy full-moon shape. In clinical trials, Casgevy eliminated pain crises in most patients.
The FDA approved the treatment for people 12 years and older.
“Sickle cell disease is a rare, debilitating and life-threatening blood disorder with significant unmet need, and we are excited to advance the field especially for individuals whose lives have been severely disrupted by the disease,” said Dr. Nicole Verdun, director of the Office of Therapeutic Products within the FDA’s Center for Biologics Evaluation and Research, in a statement.
“Gene therapy holds the promise of delivering more targeted and effective treatments, especially for individuals with rare diseases where the current treatment options are limited,” Verdun added.
While the treatment itself is administered only once, the whole process takes months. Blood stem cells are extracted and isolated before being sent to Vertex’s lab, where they’re genetically modified. Once ready, patients receive chemotherapy for a few days to clear out the old cells and make room for the new ones. After the new cells are infused, recipients spend weeks in the hospital recovering.
Vertex will take the lead on launching the drug and estimates about 16,000 people with severe cases of sickle cell will be eligible.
Even among the people who could benefit the most, analysts worry few will clamor for a treatment that takes months to complete, carries the risk of infertility and could be cost prohibitive. Vertex said in a regulatory filing Friday it will charge $2.2 million per patient for the treatment.
“We believe the price of medicine to reflect the value that it brings, and the value that this brings is a one-time therapy for potentially a lifetime of cure,” Vertex CEO Dr. Reshma Kewalramani said Friday in an interview with CNBC.
Vertex is seeing “unanimous enthusiasm” from payers, patients and physicians, because people with sickle cell have been marginalized, Kewalramani said, and the field hasn’t seen much innovation.
Because the procedure is so complex, it will be limited to certain health facilities like academic medical centers. Nine health-care facilities are ready to start administering Casgevy, Vertex said in a release, with more facilities added in the coming weeks.
Bluebird’s Lyfgenia
The FDA also on Friday approved a separate gene therapy by Bluebird Bio, called Lyfgenia that works differently than Casgevy but is administered similarly and is also intended to eliminate pain crises. That therapy was similarly approved for the treatment of sickle cell disease in people 12 years and older.
Bluebird will charge $3.1 million per patient for Lyfgenia. Shares of that company, which has a market value of just about $300 million, fell 40% Friday.
Dr. Peter Marks, director of the FDA’s Center for Biologics Evaluation and Research, estimated during a call with reporters Friday that across the two therapies approved Friday, close to 20,000 patients will be eligible for treatment.
But the FDA included a black-box warning – the strongest safety warning label – to Bluebird Bio’s Lyfgenia, noting that in rare cases the therapy can cause certain blood cancers.
The FDA added that warning after two patients who received Lyfgenia in a clinical trial died from a form of leukemia, Verdun told reporters Friday.
The agency said it’s still unclear whether Lyfgenia itself or another part of the treatment process, such as the chemotherapy, caused the cancer.
But Marks said that the FDA wants patients to be aware of all potential side effects of the entire treatment process: “It’s about the totality of the therapy that’s given,” he told reporters.
Vertex did not see similar blood cancer cases in its clinical trial, which is why it did not receive a black-box warning on its label, Verdun noted.
Both Bluebird Bio and Vertex will follow patients who receive the treatments for 15 years as part of a post-approval study. The FDA has encouraged the companies to specifically monitor for malignancies, or the presence of cancerous cells that can spread to other sites of the body.